The Eradication of Smallpox
Despite ethnic, religious, regional and political differences, every now and then people are able to set aside disagreements, look to their common humanity, and make the world a better place. Perhaps one of the greatest and most inspiring examples of such global cooperation has been the eradication of smallpox.
The Disease
Caused by either of two related viruses, Variola major and Variola minor, smallpox has been the scourge of humanity since pre-historic times. Transmitted by person-to-person contact, either through physical contact with infected material or by breathing in droplets infected with the virus, smallpox can be devastating when it takes hold in densely populated areas. In the 20th century alone, it is estimated that smallpox caused somewhere between 300 and 500 million deaths worldwide.
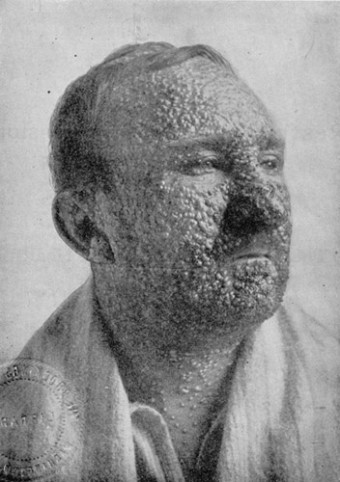
Following an incubation period of 10 to 14 days, those afflicted with the disease will develop a fever and headache before the typical maculopapular rash (a large area of discolored skin covered with small bumps) develops. This rash, which typically spreads over the face and body, may even reach the eyes where scarring sometimes leads to blindness. Although the overall mortality rate from the disease is about 30%, in children, it can reach up to 80%.
Early Eradication Efforts
Prior to the discovery of the vaccine at the end of the 18th century, eradication efforts were typically limited to inoculation – injecting a bit of the smallpox virus, taken from the pustule of an infected person, into an uninfected person with the hope of stimulating immunity. The practice, which began in China at least as early as the 10th century, was not without risk since inoculation sometimes caused deaths and even outbreaks of the disease.
The Vaccine
In the late 1790s, Dr. Edward Jenner realized that milkmaids had an apparent immunity to smallpox, and upon investigation, discovered it was due to their greater exposure to cowpox, a related but much less deadly disease. Introducing his cowpox vaccine (so named because vacca is Latin for cow) in 1796, by the mid-1800s, countries around the world had effective, organized vaccination programs.
As a result, by the early 1900s, the disease was eliminated from the US and Northern Europe. However, less-developed countries, and particularly those in warmer climates, had greater difficulty eradicating the disease due in no small part to inadequate methods of producing and/or preserving the vaccine. Luckily, by the 1950s, a freeze-dried vaccine was developed that allowed for long-term storage, even absent refrigeration.
Global Eradication Campaign
Although the Pan American Health Organization undertook an Americas-wide effort to eliminate the disease in 1950, the first global eradication program was proposed by Professor Viktor Zhdanov, the Deputy Minister of Health for the United Soviet Socialist Republic (USSR) in 1958.[1]
Arguing for an intense global effort at the 11th World Health Assembly, Professor Zhdanov convinced his fellow delegates of the efficacy and feasibility of a compulsory campaign of vaccination (and revaccination) in those countries that still had the disease.[2] His proposal was adopted at the 12th World Health Assembly in 1959, although little progress was made over the next few years.
Beginning in 1966, however, efforts at eradication intensified under the guidance of the Smallpox Eradication Unit, then led by Donald Henderson. Knowing that even with the 150 million doses of the vaccine donated by the USSR and US the vaccine supply was insufficient to vaccinate everyone, the team began to coordinate efforts around one of Zhdanov’s proposals.
Known as the Leicester system, it began by aggressively identifying infected cases and vaccinating “all known and possible contacts to seal off the outbreak from the rest of the population.” This system of “surveillance-containment” relied on “prompt identification of the disease, special notification, isolation, quarantine, disinfection measures [and] . . . the eradication of flies.”[3]
Effective, by the latter half of the 1970s, smallpox remained endemic only in a few isolated places (namely Ethiopia and Somalia) that were difficult to reach due to lack of infrastructure, famine and war. Nonetheless, in 1977 an intensive surveillance and containment program was instituted, and the last naturally occurring smallpox case was seen in Somalia in October 1977.
On May 8, 1980, the 33rd World Health Assembly declared:
That the world and its peoples have won freedom from smallpox, which was a most devastating disease sweeping in epidemic form through many countries since earliest time, leaving death, blindness and disfigurement in its wake and which only a decade ago was rampant in Africa, Asia and South America.
Smallpox Today
Although the disease has been eradicated, the virus hasn’t. After an accidental exposure, infection and death from smallpox that was contracted at a laboratory in England in 1978, all known remaining stocks have been limited by international agreement to two laboratories: the Centers for Disease Control (CDC) in Atlanta and the State Research Centre of Virology and Biotechnology (VECTOR) in Koltsovo, Russia.
Many scientists today are calling for the total destruction of these remaining stockpiles, pointing to the disease’s lethality, and the fact that this would make it easier to enforce international laws against possession of the virus.
Those in favor of retaining smallpox stocks argue that they are necessary in the event future vaccines are needed. These retentionists note that: (1) it is likely terrorists or other such groups already have smallpox samples that they can weaponize; and (2) since smallpox was eradicated, children are no longer vaccinated, so now, up to 40% of the world’s population has no natural immunity.
Notably, a recent event both supports and opposes both points of view.
In an unused portion of a storage room, in a laboratory operated by the US Food and Drug Administration (FDA) on the Bethesda, Maryland campus of the National Institutes of Health (NIH), several vials of smallpox, in containers labeled simply as “variola,” were discovered by employees who were charged with packing up the room for an impending move. Since the NIH transferred the lab to the FDA in 1972, it is entirely possible the lethal virus lay there forgotten and unmonitored for 40 years.
If you liked this article, you might also enjoy our new popular podcast, The BrainFood Show (iTunes, Spotify, Google Play Music, Feed), as well as:
- Why Native Americans Didn’t Wipe Out Europeans With Diseases
- Do Vaccines Cause Autism?
- How Chickenpox Got Its Name
- Chicken Pox Is A Form Of Herpes
- The Eleven Thousand Year Old Contagious Cancer Still Multiplying Today
Bonus Facts:
- It’s been theorized that the eradication of smallpox and the rapid rise of HIV around the same time was no coincidence. Both HIV and smallpox exploit the same receptor (CCR5) and, interestingly enough, the vaccine for smallpox has been shown to provide some protection against HIV as well. Thus, when the masses suddenly stopped being commonly vaccinated for smallpox, it made it easier for HIV to spread.
- It’s believed that small pox was the first European disease that Native Americans encountered, and it was also the most deadly. Initially just one person is thought to have developed feverish symptoms on board the ship, which caused an outbreak amongst the Europeans. When they hit land, the disease spread like wildfire across the new continent. Smallpox was highly infectious because of the blisters that broke out on an infected person. As Dr. Tim Brooks explains, “Because each of those blisters is packed full of smallpox particles, then if you burst a blister, fluid will come out and large numbers of viruses will be spilt onto whatever it touches. Ten to twelve days later, his friends would be taken ill, and then ten to twelve days after that, their friends. That kind of rate means the disease spreads exponentially.”
- CDC Media Statement on Newly Discovered Smallpox Samples
- Smallpox and its Eradication (Fenner, et al)
- Smallpox and Bioterrorism
- Smallpox Vaccine: the Good, the Bad and the Ugly
- Smallpox Vials Discovered in Lab Storage Room
- Smallpox virus: crunch time for the fate of a global killer
- Smallpox (Wikipedia)
| Share the Knowledge! |
|